What is Degenerative Disc Disease and What Can You do About it?
Physical Health

Back pain is so common it’s almost inevitable. Like sprouting a gray hair, most people deal with at least one episode of low back pain by middle age. A major cause of back pain can be degenerative disc disease. Various factors, including what’s happening both inside and outside your cells, contribute to getting degenerative disc disease. A combination of wear and tear, poor nutrition in the discs, and neural changes over time lead to degenerative disc disease. In this article, we’ll get into what degenerative disc disease is and how you can treat it.
What is Degenerative Disc Disease?
To better understand degenerative disc disease, let’s discuss the umbrella term under which it lies: low back pain. Low back pain is the fifth most common reason people go to the doctor in the United States. Whether people are extremely active or relatively sedentary, healthy or unhealthy, back pain affects most people at some point in their lives. Of the many causes of back pain, degenerative disc disease is the leading cause of lower back pain and disability. One reason may be because our discs start degenerating much earlier than our bones and muscles, which we’ll go into more detail on later. Let’s start by looking at the spine.
A Brief Look at Spine Anatomy
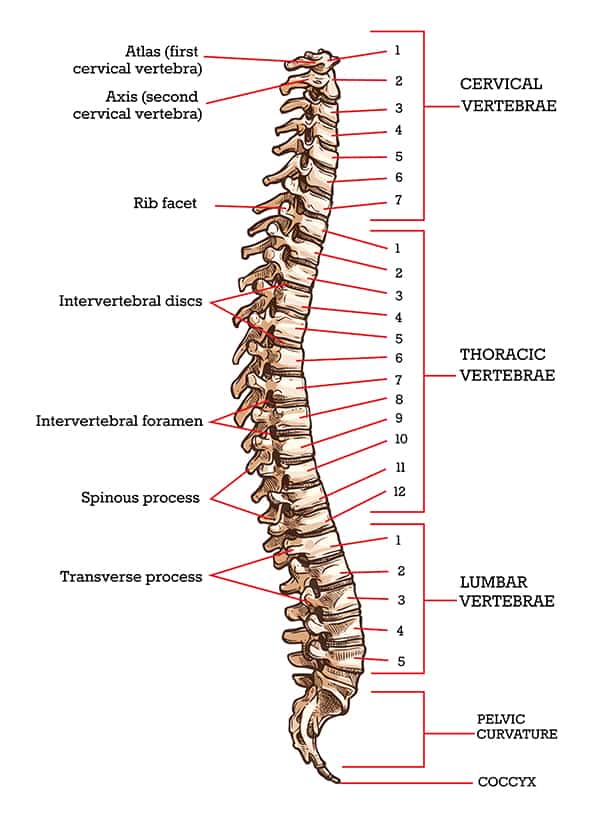
Most people are born with a spine comprised of 33 bones called vertebrae stacked on top of one another like puzzle pieces. By adulthood we typically have 24 vertebrae because the bones at the bottom of the spine fuse together. The vertebrae differ based on their location in the spine and have different functions in the neck (cervical), mid back (thoracic) and low back (lumbar) regions. While degenerative disc disease can occur in any part of the spine, we’ll focus on the most prevalent, the lumbar spine.
Each lumbar vertebra is comprised of a prominent, round body in front, a pointy spinous process in back, a transverse process on either side, the spinal canal, which houses the spinal cord, and facet joints, which articulate with the vertebra above it. When stacked together, they create the spinal column. The spinal column has 4 main functions: to support the weight of the body above the pelvis, to protect the spinal cord, to act as the central axis of the body, and to control posture and movement.
Where do Discs Come into Play?
In between the bodies of the vertebrae lie intervertebral discs, which act like soft pillows and provide flexibility and cushion to the spine. They also allow for the spine’s natural curvature, or lordosis, to absorb shock, provide stability, and carry heavier loads. Each disc is made up of three parts:
- Nucleus pulposus: The center of the disc containing the “filling”
- Annulus fibrosus: Inner and outer rings surrounding the nucleus pulposus
- Terminal endplates: Cartilage and fibrous tissue
How Discs Degenerate
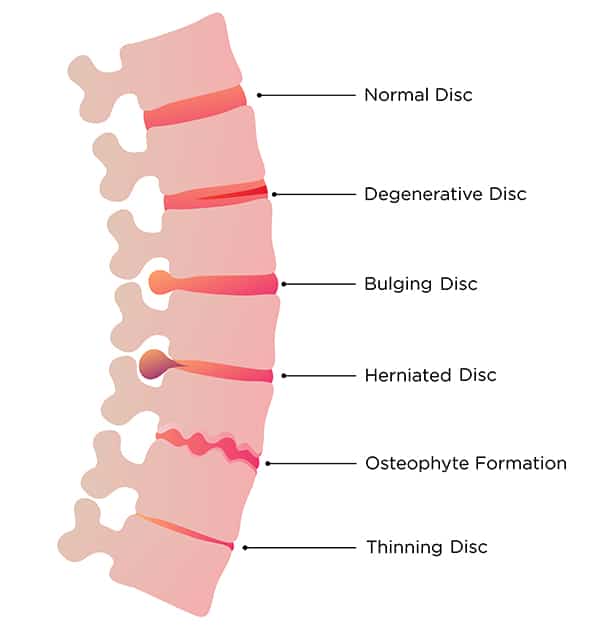
The nucleus pulposus plays the largest role in disc degeneration. A healthy nucleus pulposus is gel-like, well hydrated, and rich in proteins called proteoglycans. It creates pressure in the disc to separate the vertebra, puts tension on the surrounding rings (annulus fibrosus) to hold the disc shape, and helps evenly distribute pressure over the end plates. As we age, the nucleus pulposus loses proteoglycans, which causes the disc to become firmer, dehydrated, and more vulnerable to damage. These changes cause the disc to lose its height and pressure, which sets off a sequence of events that changes the biomechanics of the spine.
Nucleus Pulposus Over Time
| Age | Filling Consistency |
|---|---|
| Young | Jelly |
| Middle-Aged | Toothpaste |
| Older | Chalk |
Disc degeneration over time is inevitable. But many people going through it never even know it’s happening. Discs begin the degeneration process as early as adolescence, with 20% of young people showing mild symptoms. It’s when these changes cause painful and debilitating symptoms that we refer to it as degenerative disc disease, or intervertebral disc disease.
What Causes Degenerative Disc Disease?

Like many other chronic conditions, such as heart disease and diabetes, no one specific event causes degenerative disc disease. Degenerative disc disease results from a complex interaction of genetics, age, structural changes, biochemical changes, environment, trauma, and activity level over time. Three main factors lead to the progression of degenerative disc disease: wear and tear, decreased nutrition in the discs, and neural changes.
Wear and Tear
Natural disc degeneration can start as early as ages 11-16, but most people begin showing symptoms in middle age, after they have put their spines through some wear and tear. Age-related changes cause an imbalance between building tissue (anabolism) and breaking tissue down (catabolism). This changes the composition of the nucleus pulposus, leaving it dehydrated and firmer. As disc height falls, the dynamics of the extracellular matrix (area surrounding disc cells) change, causing the once perfectly functioning spine to use altered movement patterns.
Decreased Nutrition in the Discs
With age, less nutrients are supplied to the discs, causing terminal end plates to harden and calcify. Nutrient loss also causes discs to be less capable of load distribution. As one disc degenerates, it causes surrounding segments to work harder to distribute load and maintain postural stability, which accelerates degeneration of the surrounding discs. This in turn affects other structures, such as joints, ligaments and muscle.
Neural Changes
The discs in the spine are aneural (without nerves) and avascular (without blood vessels). So how do they generate so much pain? When the disc degeneration cycle progresses, a series of reactions are stimulated in which cytokines, the immune responses’ signaling cells, are secreted. An inflammatory response follows, which can cause tears in the annulus fibrosis (fissures), push the disc into nerve tissue (bulge), or even cause the nucleus pulposus to rupture and leak out (herniate). Over time, the spinal canal becomes too narrow (spinal stenosis) and compresses nerve tissue (radiculopathy), which causes pain.
Am I at risk?

If you are getting older by the day (hint: we all are!), then you are at risk of disc degeneration. Since discs begin degenerating much earlier than muscles and bones, many people who experience low back pain associated with degenerative disc disease are of working age. This may explain why degenerative disc disease is the leading cause of work-related disability. Some factors may put you at higher risk for developing degenerative disc disease. Here are a few to keep in mind:
- Age: The older the individual, the higher the risk
- Genetics: If one or more family members have been affected, you are more likely to be affected
- Gender: Men are at higher risk
- Joint laxity: Imbalances in muscle dynamics can create spinal instability
- Repetitive loading over time: Healthcare workers, foundry and forest workers, production operators, cabinet makers, truck drivers, locksmiths, bricklayers, and workers who lift, rotate, and/or bend are more at risk
- Environmental factors: Smoking, obesity, and diabetes mellitus increase the risk
- Psychosocial factors: Low socioeconomic status and depression increase the risk
- Nutritional deficiency: Poor disc nutrition accelerates degeneration
How do I know if I have Degenerative Disc Disease?
Degenerative disc disease may be present in 90% of people over age 70. So why don’t 90% of people over age 70 have severe low back pain? Many people with degenerative disc disease are asymptomatic and will never need treatment. Others have episodic bouts of pain that are treatable with conservative interventions, which is why your physician usually won’t jump right to ordering an MRI. Chances are, if you have back pain, an MRI will show some degeneration of your discs. But that won’t necessarily change the course of treatment. Managing symptoms is the priority.
Symptoms
Besides the most obvious symptom of low back pain, the next most common symptom is sciatica, or nerve type pain running down the leg. This type of pain is usually sharp and shooting and may feel numb and tingly radiating down the leg and foot. It can be on one or both sides, and can follow what are called dermatomal patterns, or areas of the leg innervated by certain nerves. Specifying the location of your symptoms can help your clinician determine what level of the spine he or she suspects is involved.
Your symptoms may be aggravated with bending, sitting, turning, coughing, sneezing, and occasionally standing. Typically, if sitting aggravates your symptoms, then standing or laying will alleviate them, and vice versa. However, in an acute case of a disc herniation, it may be painful to be in any position.
Things to Report Immediately
While degenerative disc disease symptoms may be painful, they aren’t usually dangerous. However, there are a few symptoms that require immediate evaluation by a medical professional. These can lead to rare, but potentially life-threatening complications:
- Change in bowels or bladder accompanying back pain
- Saddle anesthesia (loss of sensation in the buttocks, perineum, and inner thighs)
- Fever
- Drug abuse
- Recent trauma (car accident, fall, sports injury, etc.)
- Unrelenting pain
Diagnosis

When seeking evaluation for degenerative disc disease, you must first choose where to begin for proper medical evaluation. Your primary care physician can diagnose your condition, provide recommendations, and possibly medications to help temporarily, and this physician can provide referrals for therapy, whether this be physical therapy or occupational therapy, depending on your condition. Your primary care physician can also help you to find the most appropriate specialist for your condition -- and make this referral for you. This physician may be an orthopedic physician, a physiatrist (PM&R physician), a neurologist, or a neurosurgeon. They all specialize in differing capacities in spinal dysfunction. No matter who you choose, it’s always a good idea to know what to expect.
Your physician will ask a series of questions about your medical history, current symptoms, aggravating factors, and alleviating factors, and any medications you’ve taken for this condition. You will be asked specific questions about your pain, such as location, quality, intensity, and frequency. They may test your strength, flexibility, and range of motion. During this time, it is important to be honest: lay it all out there. Don’t be embarrassed to say you fell off the wagon with your diet, or that you haven’t left your couch since Covid-19 began. It’s important for the physician to know what’s going on in your life so you can be diagnosed accurately.
While an MRI is the main imaging technique for degenerative disc disease, it is just one of many diagnostic tools a clinician may use. Remember that more likely than not, you have disc generation if you have low back pain. Since the results of an MRI often don’t change the treatment plan for the individual, physicians typically only order them if conservative treatment fails.
What to do About it
Treatment typically starts with conservative management, which includes physical therapy, oral medications, injections, and education about understanding pain and coping mechanisms. Statistically, 80% of patients respond to physical therapy within four to six weeks.
For those who still suffer from symptoms after trying conservative care, some promising prospects are less invasive than surgery but still being studied. Restorative therapies include molecular therapy, growth factor therapy, cell therapy and gene therapy. Reconstructive methods include percutaneous IVD techniques, mechanical decompression, and biomaterial injection.
The more invasive treatments and typically last resort for symptom relief are decompression surgery, total disc replacement, and rigid fusion. While fusion protects the integrity of the segment, it may compromise other levels of the spine. It also addresses symptoms, not causes of the condition.
If you want to decrease your risk of getting degenerative disc disease, you can start by exercising. Exercise, especially when done in moderate to high volume, with low repetition and frequency, can decrease your risk of having symptoms. Along with a multitude of other health benefits, exercise will keep your postural muscles strong, spine stable, and cardiovascular system healthy.
What Not to Do
If you suffer from degenerative disc disease, don’t lay around hoping it will go away. Bedrest can make low back pain worse. After 1-2 days of rest per new episode, it is important to move your body. Your clinician will direct you on what kind of activities are safe and effective for your case.
Conclusion
Degenerating discs are about as common as getting wrinkles with age. When they become painful and debilitating, however, we call it degenerative disc disease. It is the result of a complex interplay of actions happening both inside and outside of cells, environmental factors, genes, and change over time. If you have an episode of low back pain, you may have degenerative disc disease, but don’t schedule your surgery just yet. See your physician and they will help you get back to being you!